Decent Care is responsible for the health and safety of their team members and participants. Due to the nature of the services provided there is a risk that team members and participants will be exposed to an infectious disease. Decent Care Infection Control and Prevention Policy outlines the strategies and procedures that are in place to prevent the transmission of infections between team members and participants.
The policy applies to all team members, students, volunteers, and contractors who work with participants.
Infectious agents cause disease or illness to their hosts. Infection control is the prevention of the transmission of infectious agents and managing infections if they occur. The most common forms of transmission are contact, droplet, blood borne, and air borne. Standard precautions are work practices that provide the first line approach to infection prevention, they should be adopted by all team members working with participants. Standard precautions should be applied in all settings regardless of suspected or confirmed infection status. Standard precautions are used to reduce or prevent the transmission of infectious agents and to render and maintain objects and healthcare areas as free as possible from infectious agents.
Decent Care will ensure infection control strategies and procedures are trained out to all team members. Decent Care will ensure that appropriate PPE will be supplied to team members and they are trained in its use. Decent Care will ensure that infection control strategies and procedures are regularly assessed and consistent with current best practice and relevant guidelines and standards. Records of infection control activities are maintained, including infection control training. Any incidents raised in relation to infection control issues will be reviewed and if necessary, actions will be implemented to ensure the incident does not reoccur, affected team members will be given the opportunity to debrief if required. Infection control risks will be identified; strategies will be developed and implemented for the prevention and control of healthcare associated infections.
Standard precautions include:
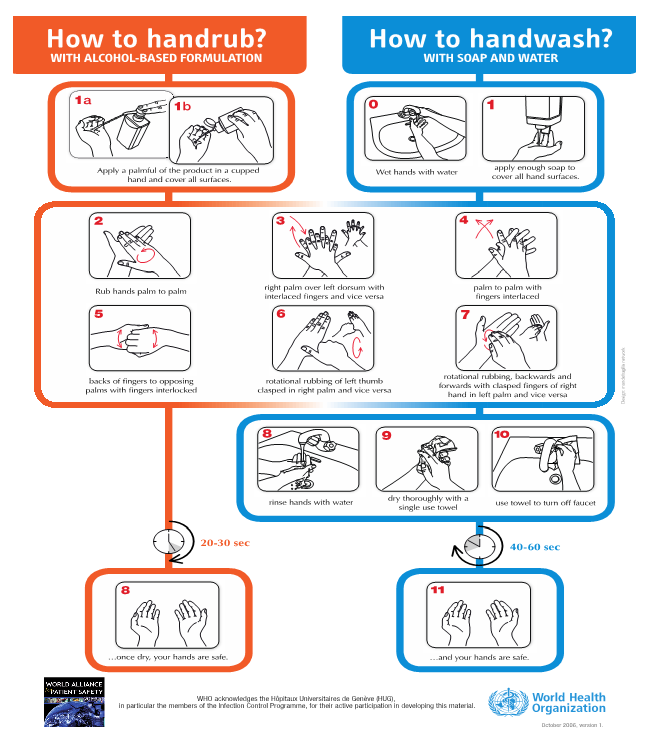
Hand hygiene is the single most effective action to reduce health care associated infections. It is the simple action of hand cleansing and when performed correctly results in a reduction of microorganisms on hands.
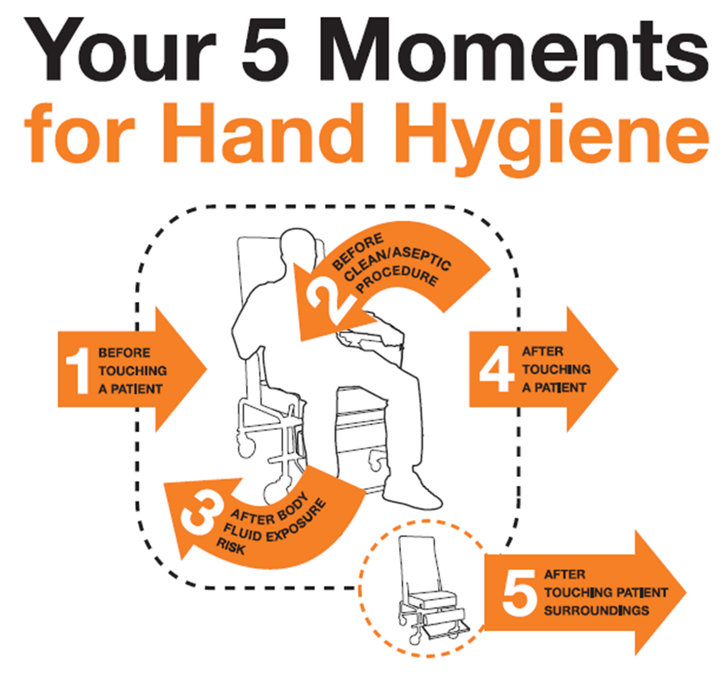
See Appendix 1 for WHO posters on how to Handrub and how to hand wash. WHO recommends using the 5 moments of hand hygiene as the guide as to when hand hygiene should be performed in a care setting.
Personal protective equipment (PPE)
All team members whom provide direct support to participants is able to access PPE from Decent Care. This is also available to participants for the duration of time of which the team member is providing support.
Personal protective equipment is equipment that provides a barrier between the team members and the participant items include:
PPE should be utilised where there is a possibility of sprays or spills or exposure to blood or body substances during a procedure. Examples may include wearing, wearing gloves when changing a dressing or changing a bed that has body fluids contaminating it. Gloves should be changed after every procedure and in between care occurring between participants. Gloves do not replace hand washing: hand washing should be completed after removing gloves. Glasses and goggles are reusable and can be wiped down after use.
Cleaning of shared participant equipment
Any equipment that is shared by participants must be wiped down with a detergent solution between use.
Respiratory hygiene and cough etiquette
Team members should cough or sneeze into a tissue or their elbow and always wash hands after this has occurred. Covering sneezes and coughs prevents people who are infected from dispersing droplets into the air where they can spread to others.
Routine environmental cleaning
All team members who support participants must ensure standard precautions are implemented throughout all settings in which support is provided to participants.
When delivering support to participants, team members are required to maintain work areas in a clean condition, regularly wipe down frequently touched surfaces with disinfectant and with warm water and mild detergent. They must keep cleaning equipment in good working order and ensure floors are in a clean condition, no signs of visible dirt and mopped/ vacuumed regularly.
Safe handling and disposal of waste and used linen safely
See Management of Waste Policy for management and disposal of waste.
Used linen should be handled carefully, to avoid spreading infectious agents into the environment or onto team members clothing. Do not carry soiled linen, take the linen basket to the bedside. Wash with hot water and detergent.
Infectious disease outbreak management
An outbreak can be defined as: "when there are more cases of infection with the same organism than would normally be expected in one area or period of time".
https://www.nhmrc.gov.au/health-advice/public-health/preventing-infection
In the event of an outbreak in a shared accommodation facility, infected participants should be isolated. Relevant medical practitioners and health authorities should be notified. Further information can be found in the government publication “The Blue Book”
Team member suspected illness and vaccination
Team Members must not present for their shift if they are known to have an infectious illness. They may return to work once they are symptom free or they have a certificate of clearance from their medical practitioner. Any team members presenting with signs and symptoms of an infectious disease may be sent home by management.
In the event of Gastroenteritis team members may not return to work until they have been symptom free for over 48 hours after all symptoms have resolved.
Participants attending day programs should remain home until well.
Consideration should be given to support workers that work within supported accommodation, day program setting where there is a risk of a splash or spill from body fluids to be vaccinated.
Recommended vaccinations include:
| High risk activities | Influenza Hepatitis A Hepatitis B |
| General community contact | Influenza |
All team members are mandated to undertake a Covid-19 vaccination process (and required booster) as per the Australian Government requirements for people who are working within the Disability Sector. All team members must provide evidence that will be copied and maintained on the relevant HR file.
In the event that a team member is exposed to body fluids appropriate treatment should be initiated immediately. Complete incident report and notify immediate supervisor. The following steps should be taken:
Mucosal Splash:
Penetrating injury/needlestick injury:
All team members who provide direct support to participants undertake infection control training, including refresher training. This training includes the use and disposal of Personal Protective Equipment (PPE). Training can be accessed through Log in (covid-19training.gov.au) Team members who work directly with participants, complete the online hand hygiene learning module located at www.hha.org.au.
Australian Commission on Safety and Quality in Health Care – Infection Prevention and Control Workbook, September 2019 Hand Hygiene Australia: www.hha.org.au